[ad_1]
In this “Ask Me Anything” (AMA) episode, Peter and Bob discuss all things related to insulin resistance by revisiting the important points made in the fascinating, yet quite technical, episode of The Drive with Gerald Shulman. They devote the entire discussion to understanding the condition known as insulin resistance, how it’s measured, how it manifests in the muscle and liver, and ultimately, what we can do about it.
If you’re not a subscriber and listening on a podcast player, you’ll only be able to hear a preview of the AMA. If you’re a subscriber, you can now listen to this full episode on your private RSS feed or on our website at the AMA #20 show notes page. If you are not a subscriber, you can learn more about the subscriber benefits here.
AMA #20 Sneak Peak:
We discuss:
- Explaining the format of this AMA: Extracting insights from Gerald Shulman’s masterclass on insulin resistance (2:00);
- The basics of insulin, defining insulin resistance (IR), and gold-standard methods of quantifying IR in the muscle (7:15);
- Practical ways to test for insulin resistance in a normal clinical setting (15:45);
- How insulin resistance manifests in the muscle (23:00);
- The biochemical block in glycogen synthesis—drivers and mechanisms resulting in insulin resistance in the muscle (30:45);
- The disparity in fat oxidation between insulin-sensitive and insulin-resistant individuals (44:45);
- The fate of the ingested carbohydrate in someone who is insulin resistant (51:00);
- The prevalence and clinical phenotype of insulin resistance (1:00:15);
- The role of exercise in mitigating and reversing insulin resistance (1:05:00);
- How insulin resistance manifests in the liver (1:09:15);
- Biggest takeaways: what we can do to mitigate and prevent insulin resistance (1:20:45); and
- More.
§
Explaining the format of this AMA: Extracting insights from Gerald Shulman’s masterclass on insulin resistance [2:00]
Peter recently did a podcast with Gerald Shulman: #140 – Gerald Shulman, M.D., Ph.D.: A masterclass on insulin resistance—molecular mechanisms and clinical implications
- Listening to that discussion was like “drinking through a fire hose” with so much info, so many mechanisms, etc.
- Today’s AMA will be designated to going through the important points of that podcast in a slower way to unlock the takeaways
- Prep for this AMA largely came from Shulman’s Banting Memorial Lecture
Questions to answer today:
How does insulin work under normal circumstances?
What does insulin resistance really mean?
How do we even measure it?
How is insulin resistance manifested in muscle?
How is it manifested in the liver?
How are those the same or different, and what are the consequences of this?
What should you do about this?
“Once you understand the consequences of this, you’ll appreciate how central this is to your health.” —Peter Attia
The basics of insulin, defining insulin resistance (IR), and gold-standard methods of quantifying IR in the muscle [7:15]
The basics of insulin
- Insulin is secreted as what’s called a pro-peptide
- The pancreas secretes something that is inactive and it gets split into insulin and C-peptide (insulin is the active thing)
- Insulin as a very anabolic (building/growing) hormone, and does the following:
- Drives glucose into muscles where it can be turned into glycogen
- Plays a role in glycogen synthesis in the liver
- Increases fatty acid uptake into fat cells
- In short: Insulin makes fat cells more fat, it makes muscle cells more glycogen rich, and it makes the liver more glycogen rich.
- It’s a pro-building hormone
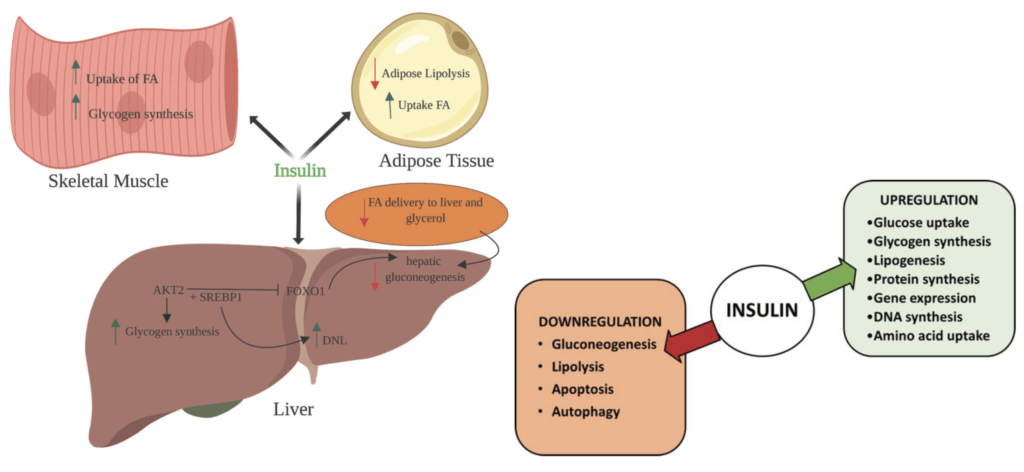
Figure 1. Effects of Insulin on Glucose & Lipid metabolism (left, 2019); Critical actions & pathways controlled by insulin (right, 2018).
Defining insulin resistance (IR) and how it’s measured
Definition:
- Insulin resistance is probably best defined as an impaired ability for insulin to do some of the things listed above
- E.g., if insulin’s job is to take glucose into a muscle so that a muscle can make glycogen, when that gets impaired, that is insulin resistance in the muscle
- However, fat cells and liver cells have a slightly different explanation/manifestation of insulin resistance
How insulin is measured (Focusing on the muscle for this discussion)
There are a couple of gold standard ways to measure and quantify insulin resistance that are done in clinical trials (i.e., not something done at the doctor’s office as part of any regular checkup)
1-Hyperinsulinemic-euglycemic clamp technique
- Using to separate IV lines…
- The plasma insulin concentration is acutely raised and maintained at 100 μU/ml by a continuous infusion of insulin.
- Meanwhile, the plasma glucose concentration is held constant at basal levels by a variable glucose infusion.
- When the steady-state (i.e., euglycemic/normal) is achieved, the glucose infusion rate equals glucose uptake by all the tissues in the body (almost exclusively into their muscles)
- This is a measure of tissue insulin sensitivity, and the more insulin sensitive you are, the higher that glucose disposal rate will be
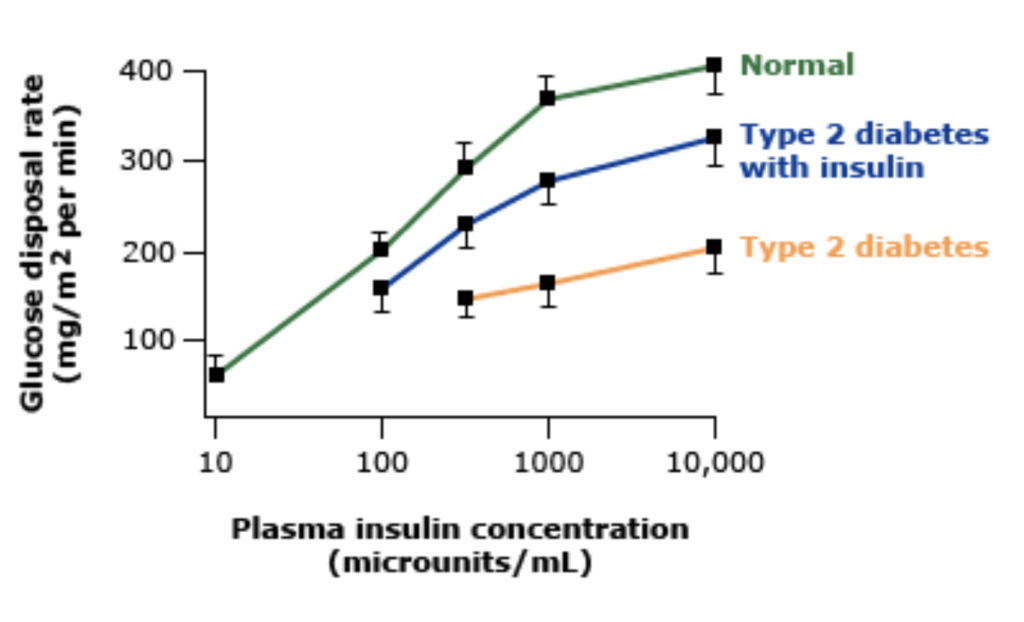
Figure 2. [UpToDate]
- The figure above is actually showing glucose disposal, not glucose
- And that’s why the more insulin-sensitive person at a fixed level of insulin requires more and more glucose to maintain glucose homeostasis
2-Insulin suppression test
- Two IV lines
- In one of them you’re infusing epinephrine, propranolol (which suppress your endogenous insulin release) as well as insulin
- in the other IV, you’re infusing glucose
- This is done until you have a steady state level of glucose and insulin
- The way this test works is kind of the opposite of the euglycemic clamp, which is you fix the level of glucose and you’re trying to see how much insulin is required to do that
- Because the steady-state insulin level is the same in all subjects, the height of the steady-state plasma glucose level provides a direct estimate of insulin resistance.
- NOTE: When Peter did this test, he got very, very hypoglycemic and it got a little dangerous
{end of show notes preview}
[ad_2]
Source link